Comorbidities and Analgesic Choice
TYLENOL® is an appropriate analgesic choice for many patients, including those with certain comorbid conditions

54%* of patients may be at risk for adverse events if their comorbidities are not considered in pain reliever recommendations.1
Consider TYLENOL®:
Appropriate for a wide range of patients, including those on aspirin heart therapy and those with a history of gastrointestinal (GI) problems or kidney dysfunction2-7
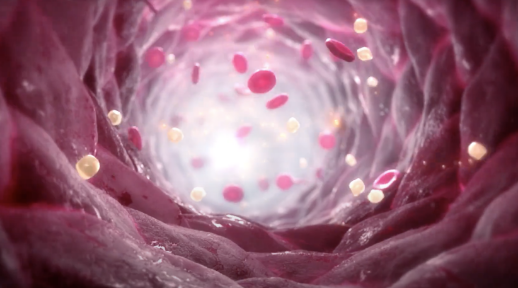
Does not increase the risk of heart attack, heart failure, or stroke the way NSAIDs such as ibuprofen or naproxen sodium can8
Does not irritate the stomach the way aspirin, naproxen sodium, or ibuprofen can3-6
References:
1. Data on file. Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division. Cross Condition Report. Fort Washington, PA; 2011.
2. Catella-Lawson F, Reilly MP, Kapoor SC, et al. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2001;345(25):1809-1817.
3. Hoftiezer JW, O’Laughlin JC, Ivey KJ. Effects of 24 hours of aspirin, Bufferin, paracetamol and placebo on normal human gastroduodenal mucosa. Gut. 1982;23(8):692-697.
4. Blot WJ, McLaughlin JK. Over the counter non-steroidal anti-inflammatory drugs and risk of gastrointestinal bleeding. J Epidemiol Biostat. 2000;5(2):137-142.
5. Naproxen. MedlinePlus. Updated March 15, 2022. Accessed March 19, 2023. https://www.nlm.nih.gov/ medlineplus/druginfo/meds/a681029.html
6. Frech EJ, Go MF. Treatment and chemoprevention of NSAID-associated gastrointestinal complications. Ther Clin Risk Manag. 2009;5(1):65-73.
7. Henrich WL, Agodoa LE, Barrett B, et al. Analgesics and the kidney: summary and recommendations to the Scientific Advisory Board of the National Kidney Foundation from an ad hoc committee of the National Kidney Foundation. Am J Kidney Dis. 1996;27(1):162-165.
8. FDA strengthens warning of heart attack and stroke risk for non-steroidal antiinflammatory drugs. US Food and Drug Administration. June 9, 2015. Accessed March 20, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-strengthens-warning-non-aspirin-nonsteroidal-anti-inflammatory#:~:text=Safety%20Announcement,a%20heart%20attack%20or%20stroke
*Percentage of consumers age 45+ who have high blood pressure, kidney disease, or are taking low-dose aspirin for heart health and, thus, may not be appropriate to use NSAIDs.