Cardiovascular Disease and Analgesic Choice
For your patients with cardiovascular disease (CVD), recommend TYLENOL® for pain
TYLENOL®: For patients with CVD, an appropriate analgesic option
Over 92 million American adults have at least 1 type of cardiovascular condition.1* When these patients need pain relief, consider TYLENOL®:
Won’t increase the risk of heart attack, heart failure, and stroke the way ibuprofen or naproxen sodium can2
Won’t interfere with aspirin heart therapy (AHT) the way ibuprofen can2
Does not have a cardiovascular risk warning on its label; over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs) do
The American Heart Association identified acetaminophen as a first-line pain-relief option for patients with, or at high risk for, cardiovascular disease3*†
TYLENOL® will not inhibit aspirin’s cardioprotective mechanism4
50 million US adults are on AHT.5 But if your patients on AHT take ibuprofen for pain, they may compromise the cardiovascular benefits.
How ibuprofen can interfere with AHT4
Ibuprofen competes for the same binding site on platelets’ cyclooxygenase-1 (COX-1) enzyme
This can interfere with aspirin’s ability to exert antiplatelet effects
GI bleeding considerations, too
Adding any NSAID to AHT can increase the risk of GI bleeding6-8
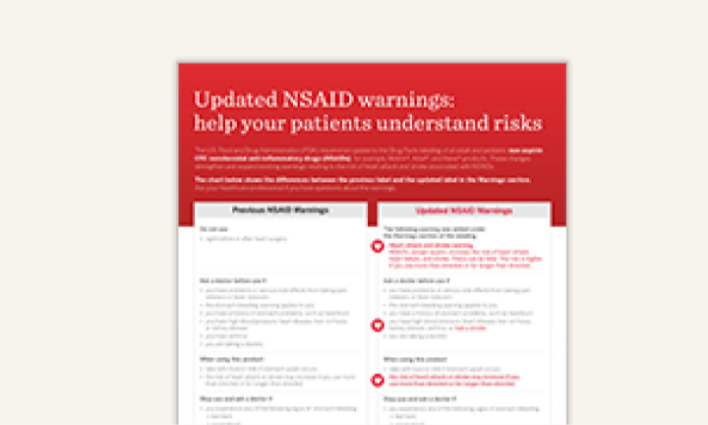
NSAID cardiovascular label warnings: Help your patients understand risks
In 2015, the US Food and Drug Administration (FDA) required an update to the Drug Facts labeling of all adult and pediatric non-aspirin OTC NSAIDs—for example, Motrin®, Advil®, and Aleve® products. These updates strengthened and expanded existing warnings relating to the risk of heart attack and stroke associated with NSAIDs.2
Order practice resources
Get complimentary samples and coupons, condition-focused patient education resources, and more.
CVD=cardiovascular disease; GI=gastrointestinal; OA=osteoarthritis
*Cardiovascular disease in reference was defined as hypertension, myocardial infarction, angina pectoris, heart failure, or stroke.
†When symptoms are not controlled by nonpharmacologic approaches.
References
1. Benjamin EJ, Blaha MJ, Chiuve S, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
2. FDA strengthens warning of heart attack and stroke risk for non-steroidal antiinflammatory drugs. US Food and Drug Administration. June 9, 2015. Accessed March 20, 2023.
3. Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA, et al. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115(12):1634-1642.
4. Catella-Lawson F, Reilly MP, Kapoor SC, et al. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2001;345(25):1809-1817.
5. Campbell CL, Smyth S, Montalescot G, Steinhubl SR. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297(18):2018-2024.
6. Frech EJ, Go MF. Treatment and chemoprevention of NSAID-associated gastrointestinal complications. Ther Clin Risk Manag. 2009;5(1):65-73.
7. Abraham NS, Hlatky MA, Antman EM, et al; ACCF/ACG/AHA. 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: a focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;122(24):2619-2633.
8. Kovac SH, Saag KG, Curtis JR, Allison J. Association of health-related quality of life with dual use of prescription and over-the-counter nonsteroidal antiiflammatory drugs. Arthritis Rheum. 2008;59(2):227-233.
9. Rahman MM, Kopec JA, Cibere J, Goldsmith CH, Anis AH. The relationship between osteoarthritis and cardiovascular disease in a population health survey: a cross-sectional study. BMJ Open. 2013;3(5):e https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm453610.htm
